Abstract
Background
The COVID-19 pandemic may have a differential impact on mental health based on an individual's capital, i.e. resources available to maintain and enhance health. We assessed trajectories of depression and anxiety symptoms, and their association with different elements of capital.Methods
Data on 65,854 individuals (mean baseline age = 50·4 (SD = 12·0) years) from the Lifelines COVID-19 cohort were used. Baseline mental health symptoms were on average measured 4.7 (SD = 1·1) years before the first COVID-19 measurement wave, and subsequent waves were (bi)weekly (March 30─August 05, 2020). Mental health symptom trajectories were estimated using a two-part Latent Class Growth Analysis. Class membership was predicted by economic (education, income, and occupation) and person capital (neuroticism, poor health condition, and obesity) FINDINGS: Most individuals were unlikely to report symptoms of depression (80·6%) or anxiety (75·9%), but stable-high classes were identified for both conditions (1·6% and 6·7%, respectively). The stable-high depression class saw the greatest increase in symptoms after COVID, and the stable-high anxiety class reported an increase in the probability of reporting symptoms after COVID. At the first COVID-measurement, the mean number of symptoms increased compared to baseline (depression:4·7 vs 4·1; anxiety:4·3 vs 4·2); the probability of reporting symptoms also increased (depression:0·96 vs 0·65; anxiety:0·92 vs 0·70). Membership in these classes was generally predicted by less capital, especially person capital; odds ratios for person capital ranged from 1·10-2·22 for depression and 1·08-1·51 for anxiety.Interpretation
A minority of individuals, possessing less capital, reported an increase in symptoms of depression or anxiety after COVID.Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.Free full text
Increases in symptoms of depression and anxiety in adults during the initial phases of the COVID-19 pandemic are limited to those with less resources: Results from the Lifelines Cohort Study
Abstract
Background
The COVID-19 pandemic may have a differential impact on mental health based on an individual's capital, i.e. resources available to maintain and enhance health. We assessed trajectories of depression and anxiety symptoms, and their association with different elements of capital.
Methods
Data on 65,854 individuals (mean baseline age = 50·4 (SD = 12·0) years) from the Lifelines COVID-19 cohort were used. Baseline mental health symptoms were on average measured 4.7 (SD = 1·1) years before the first COVID-19 measurement wave, and subsequent waves were (bi)weekly (March 30─August 05, 2020). Mental health symptom trajectories were estimated using a two-part Latent Class Growth Analysis. Class membership was predicted by economic (education, income, and occupation) and person capital (neuroticism, poor health condition, and obesity)
Findings
Most individuals were unlikely to report symptoms of depression (80·6%) or anxiety (75·9%), but stable-high classes were identified for both conditions (1·6% and 6·7%, respectively). The stable-high depression class saw the greatest increase in symptoms after COVID, and the stable-high anxiety class reported an increase in the probability of reporting symptoms after COVID. At the first COVID-measurement, the mean number of symptoms increased compared to baseline (depression:4·7 vs 4·1; anxiety:4·3 vs 4·2); the probability of reporting symptoms also increased (depression:0·96 vs 0·65; anxiety:0·92 vs 0·70). Membership in these classes was generally predicted by less capital, especially person capital; odds ratios for person capital ranged from 1·10-2·22 for depression and 1·08-1·51 for anxiety.
Interpretation
A minority of individuals, possessing less capital, reported an increase in symptoms of depression or anxiety after COVID.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Research in context panel
Evidence before this study: We searched PubMed and Google Scholar for peer-reviewed papers published from Jan 1, 2020, to June 20, 2021, with the language restricted to English. In these databases, we paired the terms “COVID-19” and “coronavirus” with “mental health”, “anxi*”, “depress*”, “stress”, “change*”, “trajector*”, “capital”, “personality”, and “socioeconomic status”. Additionally, we searched for relevant Dutch publications and reports from the Dutch government. The existing international studies suggested an increase in mental health problems during the pandemic. Within the Netherlands, the impact of the Covid-19 pandemic on mental health was limited, but there was evidence to suggest that certain groups were more vulnerable (Klerk M de, Olsthoorn M, Plaisier I, Schaper J, (ed.). Een jaar met corona. Den Haag: Sociaal en Cultureel Planbureau, 2021). No previous studies tracked population-based trajectories of mental health outcomes that included measures both before and during the pandemic. Furthermore, none analysed how mental health trajectories differed by possession of capital.
Added value of this study: To our knowledge, this population-based longitudinal study is the first to examine trajectories of symptoms of depression and anxiety during the initial stage of the COVID-19 pandemic while accounting for pre-COVID-19 measures on mental health symptoms. Moreover, we assessed how trajectories differ based on an individual's possession of certain forms of capital.
Implications of all the available evidence: The current study shows the impact of the pandemic on depression and anxiety is limited, but individuals with less capital are at an increased risk of reporting symptoms of depression and anxiety. This suggests that these groups need additional support. Additionally, extra support should be given to those who report more mental health symptoms prior to the pandemic.
1. Introduction
The COVID-19 pandemic and public-health measures to limit further spread of the virus have not only raised concerns about general public health, but have also directly impacted several mental health outcomes, such as levels of loneliness, feelings of isolation, worries, and anxiety (Varga et al., 2021). Recent meta-analyses revealed a seven-fold increase in depression rates and a threefold increase in anxiety rates during the COVID-19 pandemic in the general population (Bueno-Notivol et al., 2021; Santabarbara et al., 2020). In the Netherlands, a cross-sectional survey showed that about a third of the individuals have experienced more complaints related to depression and anxiety during the pandemic than before (Trimbos Institute for Mental Health, 2020).
Evidence on mental health trajectories during the COVID-19 pandemic raises concerns regarding the mental health impact of the COVID-19 pandemic (Xiong et al., 2020). For example, a recent systematic review of longitudinal studies found a small increase in mental health symptoms at the onset of the pandemic compared to before the pandemic (Robinson et al., 2022). However, previous studies mostly focused on mental health within the general population and did not specifically identify individuals at risk of more severe declines in their mental health (Xiong et al., 2020). In-depth research via a representative cohort is needed to better understand which groups are particularly vulnerable (McGowan et al., 2020). This could eventually lead to more targeted care and to the development of preventive interventions (Campion et al., 2020; Trimbos Institute for Mental Health, 2020).
An important high-risk group may be individuals with limited capital, but evidence on this topic is scarce (Abel and Frohlich, 2012). Capital can be thought of as resources used to acquire or maintain good health (Bourdieu, 1986). Socially disadvantaged groups typically possess lower levels of capital, and they are already more likely to experience depression and anxiety compared to their socially advantaged counterparts (Lantz et al., 2005). It can be expected that these inequalities would only widen during the pandemic, as individuals with lower levels of capital are less likely to have the resources to cope with the stressors caused by the pandemic (World Health Organization, 2021). This may make them more susceptible to experiencing mental health problems during the pandemic (Lantz et al., 2005; Turner and Turner, 2005; Uekusa, 2018). For example, previous research has shown that individuals with less economic capital (i.e. education, income, and occupation) reported more depressive symptoms during quarantines including the start of the COVID-19 pandemic (Brooks et al., 2020; Xiong et al., 2020). Additionally, individuals with less person capital (i.e. personality – neuroticism, poor health conditions, and obesity) also typically report worse mental health outcomes (Chapman et al., 2011; Hyland et al., 2021; Smith et al., 2020).
The aim of this study is therefore (1) to assess trajectories in symptoms of depression and anxiety before and during the initial stages of the COVID-19 pandemic, and (2) to assess whether these changes in symptoms of depression and anxiety can be explained by different elements of economic (education, income, and occupation) and person (personality – neuroticism, poor health conditions, and obesity) capital.
2. Methods
2.1. Study design and population
The study was embedded within the Lifelines COVID-19 sub-cohort which aims to assess the psychological and societal impacts of the COVID-19 pandemic and to investigate potential risk factors for COVID-19 within the Lifelines cohort (Intyre et al., 2021). Lifelines is a multi-disciplinary prospective population-based cohort study examining in a unique three-generation design the health and health-related behaviours of 167,729 persons living in the north of the Netherlands (Scholtens et al., 2015). It employs a broad range of investigative procedures in assessing the biomedical, socio-demographic, behavioural, physical and psychological factors which contribute to the health and disease of the general population, with a special focus on multi-morbidity and complex genetics. Lifelines data (https://www.lifelines.nl/researcher/) was linked to tax registration records held by Statistics Netherlands (CBS) (https://www.cbs.nl/en-gb). To recruit participants for the Lifelines COVID-19 sub-cohort, Lifelines emailed a digital questionnaire to all participants aged 18 years or older with a known email address. The final sample consisted of 65,854 individuals whose data were successfully linked with the CBS dataset, and participated in both the second assessment of the Lifelines cohort study and at least one of the COVID-19 questionnaires.
This study used the linked Lifelines and CBS data as baseline measure (T0) and ten measurement waves from the COVID-19 sub-cohort as follow-up measures (T1-T10). The baseline measures of mental health were assessed between 2014 and 2017; on average, this assessment occurred 4·7 years (SD 1·1 years) before T1. The COVID-19 questionnaires were initially sent out on a weekly basis, but from T6 onwards they were sent out on a biweekly basis (Intyre et al., 2021), covering the period from March 30, 2020 to August 05, 2020. Further details about the recruitment strategy and data collection can be found elsewhere for both the Lifelines cohort and the COVID-19 sub-cohort (Intyre et al., 2021).
2.2. Ethical considerations
Written informed consent was obtained from each participant prior to participating in the cohort. The Lifelines cohort study is conducted according to the conventions set forth in the Declaration of Helsinki, and it has received approval from the Medical Ethics Committee of the University Medical Center Groningen (METc approval number: 2007/152).
2.3. Measures
2.3.1. Mental health outcomes
Symptoms of depression and anxiety were measured during all waves using a self-report version of the Mini-International Neuropsychiatric Interview (MINI). The MINI is compatible with international diagnostic criteria, including the International Classification of Diseases (ICD-10) and the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (Sheehan et al., 1998). Symptoms of depression (7 items) and anxiety (6 items) were measured at each measurement wave (Appendix 1). The items used for symptoms of depression and anxiety were adequate with Cronbach's alphas of 0.74 and 0.86 at T0, respectively.
2.3.2. Elements of capital
We included three elements of economic capital, i.e. education, occupation, income, and three elements of person capital, i.e. personality – neuroticism, poor health condition, and obesity. We included education, occupation, and income because they are the most frequent measures of economic capital (Andersen et al., 2009). Person capital comprises an individual's health (poor health conditions and obesity) and personality, which are considered to be both protective and promoting regarding mental illnesses (Klein et al., 2011; Schneider-Kamp, 2021). All these measures were available at T0 (i.e., pre-COVID).
Education was assessed by asking participants about their highest attained educational level, with eight response categories. This was recoded into three categories (1) low (no education; primary education; lower or preparatory secondary vocational education; junior general secondary education), (2) intermediate (secondary vocational education or work-based learning; senior general secondary education, pre-university secondary education), and (3) high (higher vocational education; university education).
Occupation was assessed by asking participants about their occupation and the main tasks related to their occupation. CBS coded all occupations automatically according to the International Standard Classification of Occupations 08 (International Labour Organization, 2012). The resulting codes were then converted to the International Socio-Economic Index of Occupational Status. The details for generating the occupational status measures are described elsewhere (Ganzeboom and Treiman, 2003).
Income was extracted from CBS tax registration records in standardized disposable household income percentiles.
Personality – neuroticism was measured using 32 items from the Dutch NEO-PI-R (Hoekstra et al., 1996). The questionnaire contains self-reported data for four of the facet scales of neuroticism: angry -hostility, self-consciousness, impulsiveness, and vulnerability. There were eight items per facet, and the items were answered on a 5-point scale ranging from 1 (false/strongly disagree) to 5 (true/strongly agree). The authorized Dutch translation of this scale has good reliability and validity (Hoekstra et al., 1996). The Cronbach's alpha coefficient for neuroticism was 0.87. The total score of the neuroticism domain is the sum of all items from each subscale, with higher scores indicating greater levels of neuroticism.
Poor health condition was defined as the presence of at least one chronic disease. The chronic diseases included in this study were heart failure, cancer, type 2 diabetes, and respiratory illnesses, which was defined as COPD or asthma. These diseases were identified with self-reported questionnaires, and were selected based on the risk groups for COVID-19 identified by the Dutch National Institute for Public Health and the Environment (2021).
Obesity was based on body mass index (BMI), calculated as weight/height (kg/m2). Weight and height were both measured by trained staff at the Lifelines research centres. Participants were classified as obese if their BMI was ≥35 kg/m2. This cut-off was selected based on RIVM guidelines which identify individuals who are seriously overweight as a risk group for COVID-19.
2.3.3. Covariates
Information on sex and age was measured during T0.
2.4. Statistical analysis
First, we described the baseline characteristics of the sample and compared the characteristics of those who participated in the COVID-19 sub-cohort and those who were eligible but did not participate. Second, we identified distinctive trajectories over the 11 measurement waves for the number of symptoms of both depression and anxiety with a two-part Latent Class Growth Analysis. This model simultaneously combined two growth models. The first (binary) part modelled the probability of having two or more symptoms using a longitudinal logistic regression. The cut-off point of two or more symptoms was selected because most individuals were generally “healthy” (0 or 1 symptom) throughout the study period, and changes between 0 and 1 were not considered very informative. The second (count) part estimated the expected number of symptoms assuming two or more symptoms were present with a longitudinal truncated Poisson regression. Time was modelled as categorical, so no predefined trajectory shape was assumed. Thus, each class was defined by probabilities of having two or more symptoms and the average number of symptoms (≥2) per wave. Up to 25,000 random sets of starting values were used, with the 5000 best being retained for final optimization steps. Full information maximum likelihood estimation with robust standard errors was used to account for missing data, which we assumed was missing at random. Selection of the number of classes was based on the goodness of fit indices Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and Sample Adjusted BIC (a-BIC) and the interpretability of the resulting classes.
Lastly, we assessed the association with elements of capital by predicting class membership from education, income, occupation, neuroticism, poor health condition, and obesity in the final model, adjusted for age and sex. For this, we fixed all trajectory parameters and re-ran the models with class membership as the outcome of a multinomial logistic regression. We also conducted sensitivity analyses using the individual diseases (heart failure, cancer, type 2 diabetes, and respiratory illnesses) instead of poor health condition. Data were prepared using SPSS version 25 and R version 3.6.2. Descriptive statistics were prepared using SPSS, and all other statistical analyses were performed using Mplus version 8.1. Examples of the Mplus code can be found in Appendix 2 and 3.
3. Results
3.1. Sample characteristics
Table 1 provides a summary of the baseline characteristics of both the participants and non-participants from the COVID-19 sub-cohort. Participants in the COVID-19 cohort were on average older, more often female, higher educated, had higher income and occupation, had lower neuroticism scores, and reported less symptoms of depression and anxiety compared to non-participants. The number of symptoms of depression and anxiety reported at T0 and T1 and the changes in symptoms from T0 to T1 were similar for individuals whose T0 occurred within 5 years of T1 and those with longer follow-up (Appendix 4).
Table 1
Description of the baseline characteristics of the eligible participants who participated in the Lifelines COVID-19 cohort, and those who did not participate.
| Participants in COVID-19 cohort | Non-participants in COVID-19 cohort | |||
|---|---|---|---|---|
| Variables | Mean (SD) or n (%) | N | Mean (SD) or n (%) | N |
| Age (years) | 50·4 (12·0) | 65854 | 48·3 (12·0) | 46078 |
| Gender | 65854 | 46078 | ||
| Male | 26232 (39·8%) | 20331 (44·1%) | ||
| Female | 39622 (60·2%) | 25747 (55·9%) | ||
| Education | 59228 | 38764 | ||
| Low | 15474 (26·1%) | 13127 (33·9%) | ||
| Intermediate | 21933 (37·0%) | 14301 (36·9%) | ||
| High | 21821 (36·8%) | 11336 (29·2%) | ||
| Occupation | 48·6 (20·8) | 63420 | 44·2 (20·8) | 43577 |
| Income | 58·6 (26·7) | 63637 | 55·3 (26·8) | 44150 |
| Neuroticism | 46·2 (12·6) | 58995 | 47·6 (12·7) | 38978 |
| Poor health condition | 15033 (22·8%) | 65823 | 10910 (23·7%) | 45997 |
| Obesity | 2466 (3·8%) | 65466 | 1831 (4·0%) | 45372 |
| Number of depressive symptoms | 0·5 (1·1) | 55714 | 0·6 (1·2) | 34808 |
| Number of anxious symptoms | 1·0 (1·7) | 55715 | 1·1 (1·8) | 34808 |
3.2. Trajectories in symptoms of depression and anxiety
For both symptoms of depression and anxiety, the best fitting model had four classes (Table 2 ). For both sets of models adding a fifth class resulted in estimation issues. Additionally, the new classes were not very informative as they were simply adding more details about individuals without symptoms, and we were generally more interested in identifying populations that were experiencing symptoms.
Table 2
Comparison of goodness of fit criteria for the two-part models of symptoms of depression and anxiety.
| Model | AIC | BIC | a-BIC | Entropy |
|---|---|---|---|---|
| Depression | ||||
| 1 class | 397233·458 | 397433·541 | 397363·624 | 1 |
| 2 classes | 332499·482 | 332908·741 | 332765·730 | 0·889 |
| 3 classes | 325335·022 | 325953·458 | 325737·353 | 0·844 |
| 4 classes | 323893·241 | 324720·854 | 324431·654 | 0·821 |
| 5 classesa | 322909·161 | 323945·951 | 323583·657 | 0·800 |
| Anxiety | ||||
| 1 class | 581296·309 | 581496·387 | 581426·471 | 1 |
| 2 classes | 497921·424 | 498330·675 | 498187·664 | 0·858 |
| 3 classes | 488608·662 | 489227·085 | 489010·980 | 0·797 |
| 4 classes | 486595·827 | 487423·423 | 487134·223 | 0·790 |
| 5 classesa | 485513·657 | 486550·426 | 486188·132 | 0·737 |
The depressive symptom trajectories were fairly stable, and the first class (n = 1·6%) was the only class that showed an increase in the mean number of symptoms of depression at the start of the COVID-19 pandemic (Fig. 1 and Appendix 5). In this stable-high group the mean number of symptoms of depression increased from T0 to T1 (4·1 and 4·7, respectively), and the probability of reporting symptoms also increased (0·65 and 0·96, respectively). These increases persisted throughout follow-up. While the mean number of symptoms did not increase in the second (n = 13·2%) or third (n = 4·7%) class, these groups were more likely to report symptoms during T1 than T0 (0·41 vs 0·26 and 0·78 vs 0·43, respectively). However, this increase did not persist in the second class. The fourth class was unlikely to report symptoms of depression at any measurement wave.
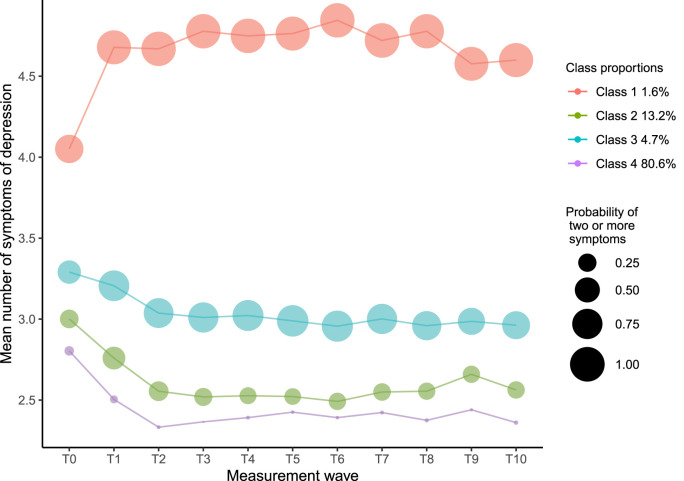
Latent class two-part trajectories for symptoms of depression over time (n = 65,818). The first part estimates the probability of reporting ≥2 symptoms (indicated by size of the points), and the second part estimates the expected number of symptoms assuming two or more symptoms are present (indicated by the lines).
For anxiety, the first class (n = 6·7%) reported an increase in the mean number of symptoms at the start of the pandemic, and the other classes reported a decrease in mean number of symptoms (Fig. 2 and Appendix 6). In the stable-high first class both the mean number of symptoms and probability of reporting symptoms increased from T0 to T1 (4·2 vs 4·3 and 0·70 vs 0·92, respectively). The probability of reporting symptoms remained fairly stable, but the mean number of symptoms of anxiety slightly decreased throughout follow-up. In the second class (n = 10·5%), both the mean number of symptoms and probability of reporting symptoms generally decreased throughout follow-up. The third class (n = 6·9%) initially showed a decrease in both the mean number of symptoms of anxiety and the probability of reporting symptoms, but both of these increased after T3. Again, the fourth class (n = 75·9%) was unlikely to report symptoms of anxiety at any measurement wave.
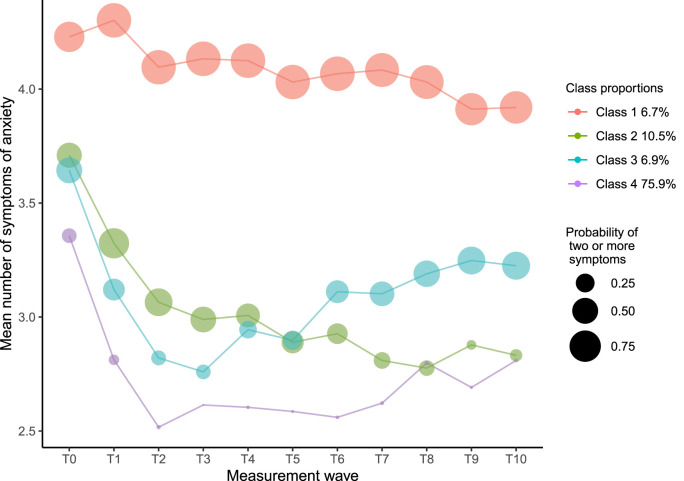
Latent class trajectories for symptoms of anxiety over time (n = 65,806). The first part estimates the probability of reporting ≥2 symptoms (indicated by size of the points), and the second part estimates the expected number of symptoms assuming two or more symptoms are present indicated by the lines.
3.3. Associations between the elements of capital and trajectories of depression
Table 3 provides the measure of the strength of the association between the various elements of capital and symptoms of depression and anxiety. For economic capital, low education increased the odds of being in the third class (odds ratio, OR (95%confidence interval, CI): 1·28 (1·04; 1·68)). Furthermore, higher income decreased the odds of being in the first class (OR (95%CI): 0·91 (0·87; 0·97)) and higher occupation increased the odds of being in the third class (OR (95%CI): 1·06 (1·06; 1·07)). Individuals with less person capital were consistently more likely to be in the first, second, or third class. The odds of being in the first class compared to the fourth class was increased by having higher neuroticism scores, poor health conditions, and obesity (OR (95%CI): 1·10 (1·09; 1·11), 1·96 (1·60; 2·54), and 2·22 (1·60; 3·42), respectively). In the sensitivity analyses, using the separate illnesses, having a respiratory illness was the only disease that increased the odds of being in the first, second, and third class (OR (95%CI): 1·89 (1·51; 2·38), 1·47 (1·32; 1·63), and 1·62 (1·39; 1·90), respectively) (Appendix 7).
Table 3
Associations between elements of capital and trajectories of symptoms of depression (n = 48,906) and anxiety (n = 48,900): results from multinomial class membership prediction modelsa, which use class 4 (low-stable) as reference class.
| Adjustedb, odds ratio (95% confidence interval) | |||
|---|---|---|---|
| Class 1 | Class 2 | Class 3 | |
| Depression | |||
| Elements of economic capital | |||
| Educationc | |||
| Intermediate | 1·22 [0·95; 1·71] | 0·98 [0·89; 1·12] | 1·18 [1·00; 1·46] |
| Low | 1·34 [0·98; 2·02] | 1·00 [0·88; 1·18] | 1·28 [1·04; 1·68] |
| Incomed | 0·91 [0·87; 0·97] | 0·97 [0·95; 1·00] | 0·98 [0·95; 1·02] |
| Occupationd | 1·02 [0·96; 1·10] | 1·03 [1·00; 1·06] | 1·06 [1·02; 1·11] |
| Elements of person capital | |||
| Neuroticismd | 1·10 [1·09; 1·11] | 1·05 [1·05; 1·06] | 1·06 [1·06; 1·07] |
| Poor health conditiond | 1·96 [1·60; 2·54] | 1·39 [1·27; 1·56] | 1·50 [1·31; 1·80] |
| Obesitye | 2·22 [1·60; 3·42] | 1·30 [1·07; 1·67] | 2·17 [1·74; 2·90] |
| Anxiety | |||
| Elements of economic capital | |||
| Educationc | |||
| Intermediate | 1·03 [0·92; 1·16] | 1·02 [0·92; 1·14] | 0·86 [0·75; 0·99] |
| Low | 1·09 [0·94; 1·26] | 1·08 [0·94; 1·24] | 0·75 [0·62; 0·91] |
| Incomed | 0·96 [0·94; 0·98] | 0·98 [0·96; 1·00] | 0·96 [0·94; 0·99] |
| Occupationd | 1·06 [1·03; 1·09] | 1·06 [1·03; 1·09] | 1·05 [1·01; 1·09] |
| Elements of person capital | |||
| Neuroticismd | 1·08 [1·08; 1·09] | 1·05 [1·05; 1·05] | 1·06 [1·06; 1·07] |
| Poor health conditiond | 1·51 [1·36; 1·67] | 1·22 [1·10; 1·34] | 1·22 [1·08; 1·39] |
| Obesitye | 1·48 [1·23; 1·79] | 1·18 [0·96; 1·45] | 1·17 [0·90; 1·53] |
3.4. Associations between the elements of capital and trajectories of anxiety
For economic capital, the odds of being in the third class was increased by higher occupation (OR (95%CI): 1·05 (1·01; 1·09)), and decreased with intermediate education, low education, and higher income (OR (95%CI): 0·86 (0·75; 0·99), 0·75 (0·62; 0·91), and 0·96 (0·94; 0·99), respectively). Higher income also decreased the odds of being in the first class (OR (95%CI): 0·96 (0·94; 0·98)), and higher occupation also increased the odds of being in the first and second class (OR (95%CI): 1·06 (1·03; 1·09) and 1·06 (1·03; 1·09), respectively). Again, less person capital was consistently associated with worse mental health. The odds of being in the first class was increased by having higher neuroticism scores, poor health conditions, and obesity (OR (95%CI): 1·08 (1·08; 1·09), 1·51 (1·36; 1·67), and 1.48 (1·23; 1·79), respectively). Again, having a respiratory illness was the only disease that increased the odds of being in the first, second, and third class (OR (95%CI): 1·54 (1·37; 1·73), 1·24 (1·10; 1·39), and 1·34 (1·16; 1·56), respectively) in the sensitivity analyses (Appendix 6).
4. Discussion
In this longitudinal population-based cohort study, we examined trajectories in symptoms of depression and anxiety during the initial stages of the COVID-19 pandemic. A small group of individuals reported an increase in depressive symptoms at the start of the pandemic, and this remained elevated throughout follow-up. Most groups reported less symptoms of anxiety during COVID-19 compared to the baseline measure. However, the mean number of symptoms remained relatively unchanged in a small stable-high group, and individuals within this group were more likely to report symptoms after COVID-19. Less person capital was generally associated with an increase in the odds of experiencing symptoms of depression and anxiety while for economic capital the results were mixed.
Small stable-high groups were identified for both symptoms of depression and anxiety, but otherwise the majority of the sample population did not report an increase in symptoms during the first few months of the pandemic. This seems to contradict the findings about the crisis in the study by Pierce et al. (2020). Their study, similar to the present study, prospectively investigated mental distress using the UK Household Longitudinal Study and found that mental health worsened during April 2020 (the start of the pandemic) compared to before the pandemic (Pierce et al., 2020). A recent review also found a small worsening of mental health in March–April 2022 (Robinson et al., 2022). However, this review showed that by July 2020 mental health symptoms were comparable to pre-pandemic levels. This seems largely in line with the findings of our study (Robinson et al., 2022). Our findings may also be partially explained by the fact that our sample consisted of individuals from the north of the Netherlands, where COVID-19 infection rates were much lower than nationally (Varga et al., 2021). Additionally, an international comparison of mental health outcomes during the pandemic found that levels of worries and loneliness were lower in the Netherlands compared to the UK (Varga et al., 2021). This is supported by other Dutch studies, which suggests that the differences with the UK may be explained by local factors. For instance, the Dutch government's response to the pandemic together with the comparatively generous Dutch social welfare and health care systems may partly explain differences between the UK and the Netherlands (van der Velden et al., 2021). Population-based studies using Dutch data also found that the COVID-19 pandemic did not negatively affect the prevalence of anxiety and depression (Klerk et al., 2021; van der Velden et al., 2021).
The results for economic capital were mixed; membership in the stable-high groups that experienced more symptoms during the pandemic was generally predicted by less income and higher occupational status. Additionally low education was associated with both more symptoms of depression and less symptoms of anxiety. Our findings for income and the association between education and depression were in line with our expectation that individuals with less capital experience worse mental health (Daly et al., 2020). Studies from before the pandemic also typically found that less economic capital was associated with worse mental health (Nandi et al., 2009). However, our findings for occupation and the association between education and anxiety were not in line with our expectations. Our findings seem to be partly supported by a study which found that highly educated individuals reported more mental health problems (Daly et al., 2020). The mixed findings between elements of economic capital and mental health outcomes may be explained by the fact that these different elements capture different parts of its economic nature, which have unique relationships with health (Lahelma et al., 2004). Furthermore, it is plausible that the pandemic has resulted in challenges that groups with more economic capital were less likely to have previously experienced; for example, working from home may have worsened their work life balance. This would be especially true in the case of individuals who may have had to balance the extra demands from their work with less availability of childcare. It has been found that the availability of childcare and support, may also contribute to adverse mental health outcomes during the pandemic (Gibson et al., 2021).
For both depression and anxiety symptoms, results suggested that less person capital was consistently associated with worse mental health trajectories. Individuals who express more neuroticism were more susceptible to poor mental health. This is in line with evidence from before the pandemic, which found that poor health and deviant personality traits were associated with worse mental health (Nandi et al., 2009). Moreover, a study found that neuroticism predicted pandemic-related psychopathology in adults (Gamsizkan et al., 2021). Having poor health conditions and being obese predicted an increased odds of being in the groups with more mental health problems. Several studies have shown that individuals with pre-existing health conditions had higher odds of exhibiting symptoms of stress, anxiety, and depression than healthy individuals (Gamsizkan et al., 2021; Wankowicz et al., 2021). Overall, our findings demonstrate that person capital was a stronger predictor of mental health trajectories over time than economic capital. These findings confirm those reported by Roberts et al. (2007) that personality traits predict important life outcomes, e.g. mortality, better than socioeconomic status does (measured using education and occupation). Less person capital, especially neuroticism, may be robustly linked to mental health through shared genetic pathways, increased likelihood of experiencing stressful events, and subsequently more pronounced and less well-regulated emotional responses to stressful events (Lahey, 2009). While person capital was more consistently associated with worse mental health outcomes than economic capital, economic capital should not be disregarded. The relationship between the elements of capital is very complicated, and they also could interact. For example, Packard et al. (2012) found that personality traits appeared to had greater impact on mental wellbeing among individuals with limited economic resources. Additionally, the effect of having high neuroticism scores on long-term increases in depressive and anxiety symptoms can even be amplified in individuals with chronic illness and less economic resources (Vittengl, 2017).
4.1. Strengths and limitations
A major strength of this study is its longitudinal design, which includes pre-COVID-19 measures on capitals and mental health outcomes. As far as we are aware, evidence from around the world on changes in population mental health potentially attributable to the COVID-19 pandemic has been limited by the use of convenience samples without comparing these with pre-COVID baseline data. Furthermore, by using a two-part latent class growth model, we were able to identify a high-risk group of individuals who reported a consistently high level of symptoms during the pandemic. Some study limitations also need to be acknowledged. First, we were limited to the seven items of the MINI which were consistently measured across T0-T11. However, given the large number of people who do not report symptoms it is unlikely including more items would have substantially changed our overall conclusions. Second, we acknowledge that the findings are limited to the north of the Netherlands with relatively low number of cases in the region, even accounting for undiagnosed cases (Intyre et al., 2021). Therefore, results may be difficult to generalize. Third, individuals who did not participate in the Lifelines COVID-19 cohort generally had less capital and more symptoms of depression and anxiety. These differences were relatively small, but we are aware that not including these individuals may have resulted in an underestimation of the mental health impact of the COVID-19 pandemic. Fourth, there is a large period of time between T0 and T1, and individuals may have gone through various experiences, which may have affected their mental health. However, this most likely would only affect a small group of individuals, as the mean number of symptoms at T0 was fairly similar to the mean at T1. Therefore, we assume that the majority of individual's mental health status has been fairly stable. Lastly, information bias may have affected our findings because we relied on data from self-reported questionnaires. However, it is unlikely this would have had a large impact on the assessment of our outcomes because these were assessed with a very well-validated and reliable instrument, i.e. the MINI (Sheehan et al., 1997).
4.2. Implications
Our results show the impact of the initial phases of the pandemic on depression and anxiety is limited, but individuals with less capital, especially person capital, are at an increased risk of reporting symptoms of depression and anxiety. In that regard, individuals with less person capital should be offered targeted interventions that promote their resilience. For instance, clinicians can offer individuals with limited person capital additional support and education regarding their mental health and mental health literacy, which can further promote their mental health (Safieh et al., 2021). Furthermore, clinicians can suggest reliable sources for news related to the COVID-19 pandemic, as the overwhelming amount of (dis)information may act as a stressor to their patient's mental health (Safieh et al., 2021). Additionally, extra support should be given to those who report more mental health symptoms prior to the pandemic. In the present study we only focussed on the initial stage of the COVID-19 pandemic and on symptoms of depression and anxiety. Further research is needed to investigate the long-term effects of the pandemic and could include other mental health measures over time. The period covered in this study coincides with the initial surge in cases and the subsequent reopening phase within the Netherlands. Previous research demonstrated that mental health improved during this gradual reopening phase (Varga et al., 2021), and this may also explain why we found a limited impact of COVID-19 on mental health. However, since then more stringent lockdowns were implemented and these measures have been in place for a much longer period of time. These extended lockdowns are likely to have had a bigger impact on mental health, which is why further studies are needed that look at the effect of the pandemic on mental health during subsequent lockdowns.
4.3. Conclusion
During the initial stages of the COVID-19 pandemic, a minority of individuals reported an increase in symptoms of depression or anxiety. In particular, those individuals with less capital, and especially person capital, experienced more symptoms of depression and anxiety during the follow-up period, which may stress the importance of devoting more resources to prevent further deterioration of mental health for this high-risk group of individuals.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
YQ and AL conceptualized and designed this study, had full access to and verified the underlying data, carried out the analyses, drafted the initial manuscript, and reviewed and revised the manuscript. JA carried out the analyses and reviewed and revised the manuscript. SB, PO, CV, ML AdK, and SAR conceptualized, designed, and reviewed and revised the manuscript. All authors read and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Acknowledgments
The authors wish to acknowledge the services of the Lifelines Cohort Study, the contributing research centres delivering data to Lifelines, and all the study participants. The Lifelines Biobank initiative has been made possible by subsidy from the Dutch Ministry of Health, Welfare and Sport, the Dutch Ministry of Economic Affairs, the University Medical Center Groningen, University Groningen and the Northern Provinces of the Netherland.
Footnotes
Appendix ASupplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2022.07.011.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abel T., Frohlich K.L. Capitals and capabilities: linking structure and agency to reduce health inequalities. Soc. Sci. Med. 2012;74(2):236–244. [Abstract] [Google Scholar]
- Andersen I., Thielen K., Nygaard E., Diderichsen F. Social inequality in the prevalence of depressive disorders. J. Epidemiol. Community Health. 2009;63(7):575–581. [Abstract] [Google Scholar]
- Bourdieu P. Greenwood Press; New York: 1986. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. [Europe PMC free article] [Abstract] [Google Scholar]
- Bueno-Notivol J., Gracia-Garcia P., Olaya B., Lasheras I., Lopez-Anton R., Santabarbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021;21(1) [Europe PMC free article] [Abstract] [Google Scholar]
- Campion J., Javed A., Sartorius N., Marmot M. Addressing the public mental health challenge of COVID-19. Lancet Psychiatr. 2020;7(8):657–659. [Europe PMC free article] [Abstract] [Google Scholar]
- Chapman B.P., Roberts B., Duberstein P. Personality and longevity: knowns, unknowns, and implications for public health and personalized medicine. J Aging Res. 2011;2011 [Europe PMC free article] [Abstract] [Google Scholar]
- Daly M., Sutin A.R., Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol. Med. 2020:1–10. [Europe PMC free article] [Abstract] [Google Scholar]
- Gamsizkan Z., Sungur M.A., Erdemir G. How do older age, gender and risk groups affect protective behaviours and mental health in the COVID-19 pandemic? Int. J. Clin. Pract. 2021;75(6) [Europe PMC free article] [Abstract] [Google Scholar]
- Ganzeboom H.B., Treiman D.J. Advances in Cross-National Comparison. Springer; 2003. pp. 159–193. [Google Scholar]
- Gibson B., Schneider J., Talamonti D., Forshaw M. The impact of inequality on mental health outcomes during the COVID-19 pandemic: a systematic review. Canadian Psychology/Psychologie canadienne. 2021;62(1):101–126. [Google Scholar]
- Hoekstra H., Ormel J., De Fruyt F. Swets Test Services (STS); Lisse: 1996. [Google Scholar]
- Hyland P., Shevlin M., Murphy J., McBride O., Fox R., Bondjers K., Karatzias T., Bentall R.P., Martinez A., Vallieres F. A longitudinal assessment of depression and anxiety in the Republic of Ireland before and during the COVID-19 pandemic. Psychiatr. Res. 2021;300 [Europe PMC free article] [Abstract] [Google Scholar]
- International Labour Organization International standard classification of occupations 2008 (ISCO-08): structure, group definitions and correspondence tables. Int. Lab. Off. 2012 https://www.ilo.org/wcmsp5/groups/public/@dgreports/@dcomm/@publ/documents/publication/wcms_172572.pdf [Google Scholar]
- Intyre K.M., Lanting P., Deelen P., Wiersma H., Vonk J.M., Ori A.P.S., Jankipersadsing S.A., Warmerdam R., van Blokland I., Boulogne F., Dijkema M.X.L., Herkert J.C., Claringbould A., Bakker O., Lopera Maya E.A., Bültmann U., Zhernakova A., Reijneveld S.A., Zijlstra E., Swertz M., Brouwer S., van Ooijen R., Angelini V., Dekker L., Sijtsma A., Scherjon S.A., Dekens J., Mierau J.O., Boezen H.M., Franke L. The Lifelines COVID-19 Cohort: a questionnaire-based study to investigate COVID-19 infection and its health and societal impacts in a Dutch population-based cohort. BMJ Open. 2021;11(3):e044474. 10.1136/bmjopen-2020-044474. [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Klein D.N., Kotov R., Bufferd S.J. Personality and depression: explanatory models and review of the evidence. Annu. Rev. Clin. Psychol. 2011;7(1):269–295. [Europe PMC free article] [Abstract] [Google Scholar]
- Klerk M.d., Olsthoorn M., Plaisier I., Schaper J., red F.W. Sociaal en Cultureel Planbureau; Den Haag: 2021. [Google Scholar]
- Lahelma E., Martikainen P., Laaksonen M., Aittomäki A. Pathways between socioeconomic determinants of health. J. Epidemiol. Community Health. 2004;58(4):327–332. [Europe PMC free article] [Abstract] [Google Scholar]
- Lahey B.B. Public health significance of neuroticism. Am. Psychol. 2009;64(4):241–256. [Europe PMC free article] [Abstract] [Google Scholar]
- Lantz P.M., House J.S., Mero R.P., Williams D.R. Stress, life events, and socioeconomic disparities in health: results from the Americans' Changing Lives Study. J. Health Soc. Behav. 2005;46(3):274–288. [Abstract] [Google Scholar]
- McGowan M.L., Norris A.H., Bessett D. Mental health and the covid-19 pandemic. N. Engl. J. Med. 2020;383(6):508–510. [Abstract] [Google Scholar]
- Nandi A., Beard J.R., Galea S. Epidemiologic heterogeneity of common mood and anxiety disorders over the lifecourse in the general population: a systematic review. BMC Psychiatr. 2009;9(1):31. [Europe PMC free article] [Abstract] [Google Scholar]
- National Institute for Public Health and the Environment Risk groups and COVID-19. 2021. https://www.rivm.nl/en/coronavirus-covid-19/risk-groups
- Packard C.J., Cavanagh J., McLean J.S., McConnachie A., Messow C.-M., Batty G.D., Burns H., Deans K.A., Sattar N., Shiels P.G., Velupillai Y.N., Tannahill C., Millar K. Interaction of personality traits with social deprivation in determining mental wellbeing and health behaviours. J. Publ. Health. 2012;34(4):615–624. [Abstract] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatr. 2020;7(10):883–892. 10.1016/S2215-0366(20)30308-4. [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Roberts B.W., Kuncel N.R., Shiner R., Caspi A., Goldberg L.R. The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspect. Psychol. Sci. 2007;2(4):313–345. [Europe PMC free article] [Abstract] [Google Scholar]
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022;296:567–576. [Europe PMC free article] [Abstract] [Google Scholar]
- Safieh J., Broughan J., McCombe G., McCarthy N., Frawley T., Guerandel A., Lambert J.S., Cullen W. International Journal of Mental Health and Addiction, No Pagination Specified-No Pagination Specified. 2021. [Europe PMC free article] [Abstract] [Google Scholar]
- Santabarbara J., Lasheras I., Lipnicki D.M., Bueno-Notivol J., Perez-Moreno M., Lopez-Anton R., De la Camara C., Lobo A., Gracia-Garcia P. Prevalence of anxiety in the COVID-19 pandemic: an updated meta-analysis of community-based studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2020;109 [Europe PMC free article] [Abstract] [Google Scholar]
- Schneider-Kamp A. Health capital: toward a conceptual framework for understanding the construction of individual health. Soc. Theor. Health. 2021;19(3):205–219. [Europe PMC free article] [Abstract] [Google Scholar]
- Scholtens S., Smidt N., Swertz M.A., Bakker S.J., Dotinga A., Vonk J.M., van Dijk F., van Zon S.K., Wijmenga C., Wolffenbuttel B.H., Stolk R.P. Cohort Profile: LifeLines, a three-generation cohort study and biobank. Int. J. Epidemiol. 2015;44(4):1172–1180. [Abstract] [Google Scholar]
- Sheehan D.V., Lecrubier Y., Harnett Sheehan K., Janavs J., Weiller E., Keskiner A., Schinka J., Knapp E., Sheehan M.F., Dunbar G.C. The validity of the Mini international neuropsychiatric interview (MINI) according to the SCID-P and its reliability. Eur. Psychiatr. 1997;12(5):232–241. [Google Scholar]
- Sheehan D.V., Lecrubier Y., Sheehan K.H., Amorim P., Janavs J., Weiller E., Hergueta T., Baker R., Dunbar G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatr. 1998;59(Suppl. 20):22–33. quiz 34-57. [Abstract] [Google Scholar]
- Smith L., Jacob L., Yakkundi A., McDermott D., Armstrong N.C., Barnett Y., Lopez-Sanchez G.F., Martin S., Butler L., Tully M.A. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: a cross-sectional study of UK-based respondents. Psychiatr. Res. 2020;291 [Europe PMC free article] [Abstract] [Google Scholar]
- Trimbos Institute for Mental Health Neerslachtiger, meer slaapproblemen en gedachten aan de dood door corona [More depressed, more sleeping problems and thoughts of death from coronavirus] 2020. https://www.trimbos.nl/actueel/nieuws/bericht/neerslachtiger-meer-slaapproblemen-en-gedachten-aan-de-dood-door-corona?utm_medium=email&utm_source=newsletter&utm_campaign=nieuwsflits_2009&utm_content=nieuws&utm_term=corona%3B%2520mentale%2520gezondheid
- Turner H.A., Turner R.J. Understanding variations in exposure to social stress. Health (London) 2005;9(2):209–240. [Abstract] [Google Scholar]
- Uekusa S. Rethinking resilience: bourdieu's contribution to disaster research. Resilience. 2018;6(3):181–195. [Google Scholar]
- Varga T.V., Bu F., Dissing A.S., Elsenburg L.K., Bustamante J.J.H., Matta J., van Zon S.K.R., Brouwer S., Bültmann U., Fancourt D., Hoeyer K., Goldberg M., Melchior M., Strandberg-Larsen K., Zins M., Clotworthy A., Rod N.H. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and Northern Europeans. The Lancet Regional Health - Europe. 2021;2:100020. 10.1016/j.lanepe.2020.100020. [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- van der Velden P.G., Hyland P., Contino C., von Gaudecker H.M., Muffels R., Das M. Anxiety and depression symptoms, the recovery from symptoms, and loneliness before and after the COVID-19 outbreak among the general population: findings from a Dutch population-based longitudinal study. PLoS One. 2021;16(1) [Europe PMC free article] [Abstract] [Google Scholar]
- Vittengl J.R. Who pays the price for high neuroticism? Moderators of longitudinal risks for depression and anxiety. Psychol. Med. 2017;47(10):1794–1805. [Abstract] [Google Scholar]
- Wankowicz P., Szylinska A., Rotter I. The impact of the COVID-19 pandemic on psychological health and insomnia among people with chronic diseases. J. Clin. Med. 2021;10(6) [Europe PMC free article] [Abstract] [Google Scholar]
- World Health Organization . World Health Organization; 2021. [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. [Europe PMC free article] [Abstract] [Google Scholar]
Full text links
Read article at publisher's site: https://doi.org/10.1016/j.jpsychires.2022.07.011
Read article for free, from open access legal sources, via Unpaywall:
https://pure.rug.nl/ws/files/233393119/1_s2.0_S0022395622003752_main.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/134083537
Article citations
Temporal dynamics of socioeconomic inequalities in depressive and anxiety symptoms during the COVID-19 pandemic: a scoping review.
Front Public Health, 12:1397392, 03 Jul 2024
Cited by: 0 articles | PMID: 39022423 | PMCID: PMC11252079
Review Free full text in Europe PMC
Sleep Duration on Workdays Is Correlated with Subjective Workload and Subjective Impact of High Workload on Sleep in Young Healthy Adults.
Brain Sci, 13(5):818, 18 May 2023
Cited by: 2 articles | PMID: 37239290 | PMCID: PMC10216395
Longitudinal dynamics of depression in risk groups of older individuals during the COVID-19 pandemic.
Front Epidemiol, 3:1093780, 13 Feb 2023
Cited by: 1 article | PMID: 38455897 | PMCID: PMC10911044
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort.
Med J Aust, 214(10):462-468, 26 Apr 2021
Cited by: 64 articles | PMID: 33899939 | PMCID: PMC8207103
Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis.
Lancet Psychiatry, 8(5):405-415, 24 Mar 2021
Cited by: 119 articles | PMID: 33773109 | PMCID: PMC8824360
Mental and physical health among the French population before and during the first and second COVID-19 lockdowns: Latent class trajectory analyses using longitudinal data.
J Affect Disord, 309:95-104, 19 Apr 2022
Cited by: 12 articles | PMID: 35452759 | PMCID: PMC9015949
COVID-19 Quarantine-Related Mental Health Symptoms and their Correlates among Mothers: A Cross Sectional Study.
Matern Child Health J, 25(5):695-705, 17 Nov 2020
Cited by: 21 articles | PMID: 33201448 | PMCID: PMC7670014
Funding
Funders who supported this work.

 ,1
,1 