Abstract
Background and purpose
Length of hospital stay after hip and knee arthroplasty is about 1 day in Denmark with few patients discharged on the day of surgery. Hence, a protocol for multicenter implementation of discharge on day of surgery has been instituted. We aimed to describe the implementation of outpatient hip and knee arthroplasty in a multicenter public healthcare setting.
Methods
We performed a prospective multicenter study from 7 public hospitals across Denmark. Patients were screened using well-defined in- and exclusion criteria and were discharged on day of surgery when fulfilling functional discharge criteria. The study period was from September 2022 to February 2023 with variable start of implementation. Data from the same centers in a 6-month period before the COVID pandemic from July 2019 to December 2019 was used for baseline control.
Results
Of 2,756 primary hip and knee arthroplasties, 37% (95% confidence interval [CI] 35–39) were eligible (range 21–50% in centers) and 52% (range 24–62%) of these were discharged on day of surgery. 21% (CI 20–23) of all patients (eligible and non-eligible) were discharged on day of surgery with a range of 10–31% within centers. This was an additional 15% (CI 13–17, P < 0.001) compared with patients discharged in the control period (6% in 2019).
Conclusion
We found it possible to perform outpatient hip and knee replacement in 21% of patients in a public healthcare setting, probably to be increased with further center experience.
There have been significant developments in hip and knee arthroplasty during the past decades with the introduction of fast-track protocols resulting in a reduction in postoperative length of hospital stay (LOS), postoperative morbidity, and costs [1-5]. Safe outpatient arthroplasty with discharge on day of surgery may be the ultimate goal of fast-track arthroplasty [6].
Previous single-center studies have shown the potential to discharge patients on the day of surgery after primary total hip arthroplasty (THA), total knee arthroplasty (TKA), and unicompartmental knee arthroplasty (UKA) [7-10]. Although selective use of outpatient surgery in individual centers has been shown to be feasible, the use of outpatient surgery on a national level is low [11,12]. Therefore, the study group designed a detailed protocol for the implementation of outpatient surgery in a multicenter collaboration across all regions in Denmark [13].
Hence, the aim of our study was to investigate the implementation of discharge on the day of surgery after primary hip and knee arthroplasty in a multicenter setting during the first 6-month study period.
Methods
Study design
The study was designed as a prospective multicenter cohort study. All reporting was performed according to the REporting of studies Conducted using Observational Routinely-collected Data (RECORD) guideline [14].
Setting
“The Center for Fast-track Hip and Knee Replacement” is a multicenter collaboration consisting of 8 public arthroplasty centers across all 5 regions in Denmark, covering approximately 40% of the annual number of hip and knee arthroplasties in Denmark [9,15]. Only 3 of the 8 centers had previous experience with use of outpatient surgery before the study period. An educational program was introduced supporting that all centers followed the same protocol [13]. The study period was from September 1, 2022, to February 28, 2023, with centers labelled A–G. 1 center (Hospital Unit West, Gødstrup) did not participate because of major logistical changes due to transfer to a new hospital site and therefore did not include patients. Furthermore, 4 of the centers were only ready to start inclusion from October 1, 2022.
Study population
The study population included patients receiving a primary elective THA, TKA, or UKA and included in the REDCap database at the 7 study centers in the implementation period. Patients were included after informed consent. The informed consent was in writing and necessary in order to gain full access to patient files and to send out questionnaires to the patients. Inclusion and exclusion criteria for planned outpatient surgery are presented in Table 1. Patients were discharged on day of surgery if fulfilling predefined discharge criteria (Table 2). The data completeness on center level is provided in Table 3 (see Appendix).
Table 1.
Inclusion and exclusion criteria for planned discharge on day of surgery
| Inclusion criteria |
|
| Exclusion criteria |
|
CFS = Clinical Frailty Scale [25].
This criterion was inadvertently omitted from the protocol paper but has consistently been applied across all centers.
Table 2.
Criteria for discharge on day of surgery
| Activity level |
|
| Postoperative nausea and vomiting |
|
| Pain |
|
| Postoperative bleeding |
|
EWS = national implemented Early Warning Score systems based on NEWS2 from the Royal College of Physicians [26].
Table 3.
Data completeness on center level
| Number of surgeries, n (%) | Sept. | Oct. | 2022 | 2023 | |||
|---|---|---|---|---|---|---|---|
| Nov. | Dec. | Jan. | Feb. | Total | |||
| Hospital A | |||||||
| according to department | – | 26 | 54 | 40 | 70 | 41 | 231 |
| registered in REDCap | – | 7 (27) | 22 (41) | 20 (50) | 38 (54) | 21 (51) | 108 (47) |
| Hospital:B | |||||||
| according to department | 57 | 43 | 67 | 50 | 89 | 58 | 364 |
| registered in REDCap | 21 (37) | 39 (91) | 63 (94) | 43 (86) | 78 (88) | 56 (97) | 300 (82) |
| Hospital C | |||||||
| according to department | 114 | 161 | 160 | 114 | 192 | 147 | 888 |
| registered in REDCap | 71 (62) | 140 (87) | 149 (93) | 100 (88) | 183 (95) | 135 (92) | 778 (88) |
| Hospital D | |||||||
| according to department | – | 81 | 100 | 55 | 83 | 64 | 393 |
| registered in REDCap | – | 42 (52) | 83 (83) | 43 (78) | 75 (90) | 59 (92) | 302 (77) |
| Hospital E | |||||||
| according to department | 60 | 150 | 174 | 129 | 168 | 116 | 797 |
| registered in REDCap | 15 (25) | 53 (35) | 70 (40) | 80 (62) | 114 (68) | 86 (74) | 418 (52) |
| Hospital F | |||||||
| according to department | 70 | 60 | 71 | 48 | 68 | 62 | 379 |
| registered in REDCap | 69 (99) | 56 (93) | 65 (92) | 43 (90) | 63 (93) | 61 (98) | 357 (94) |
| Hospital G | |||||||
| according to department | – | 102 | 167 | 116 | 176 | 127 | 687 |
| registered in REDCap | – | 8 (7.8) | 102 (61) | 110 (95) | 160 (91) | 113 (89) | 493 (72) |
Patients eligible for outpatient surgery were scheduled with intended start of surgery before 1 pm. (Figure 1).
Figure 1.
Flowchart.
A historic control cohort with data on the number of outpatient procedures from the study centers in a 6-month period from July 1, 2019, to December 31, 2019 was used for comparison.
Deviation from study protocol
The focus of our study was to document and describe the implementation process following the detailed protocol designed by the study group prior to the implementation process.
We occasionally noticed a discrepancy in the exclusion criteria published in the protocol paper and those used in practice. The exclusion criterion “no adult present at home during the initial postoperative night” is not mentioned in the published protocol, and our study therefore deviates from study protocol regarding this criterion.
Data sources
Data was prospectively collected by dedicated research staff at the individual study sites with physician back-up if necessary and stored online in a REDCap database in collaboration with the Open Patient data Explorative Network (OPEN) in Odense University Hospital. The database includes patient-reported data as well as detailed data on patient comorbidities and medications collected prospectively by research staff [13].
Data on the historical baseline control group was obtained from the Danish National Patient Registry (DNPR), which contains specific procedure codes, diagnosis codes as well and discharge dates from all hospitalizations since 1977 [15].
Statistics
A preliminary power calculation was performed to ensure the feasibility of the study within the planned study period. To detect a 10-percentage point increase in discharge on the day of surgery, we required a sample size of 266 patients in each group, ensuring a power of 90% and an alpha level of 5%, and this was fully achieved with a 6-month study period [13].
A before-and-after design was used, and outcomes presented as proportions with 95% confidence intervals (CI). An estimate of the intervention effect was quantified through the measurement of the difference in proportions using Stata Statistical Software: Release 18 (StataCorp LLC, College Station, TX, USA).
Ethics, registration, funding, and disclosures
The study was preregistered in the Region of Southern Denmark and approval for data storage and management of study-associated data was obtained. The study was also registered on ClinicalTrials.gov (NCT05613439).
Treatment of eligible patients for outpatient surgery was standard of care at the participating centers according to the described protocol [13] and ethical approval was therefore not required.
“The Center for Fast-track Hip and Knee Replacement” collaboration [15] was funded in 2021 from the NOVO Nordisk Foundation (Grant number: NNF21SA0073760) to support the overall fast-track project, including research staff at all centers, data management and follow-up on complications. Furthermore, salary for the PhD student (OD) was funded from the Candy’s Foundation, University of Southern Denmark and Region of Southern Denmark. HK and KG are members of the Zimmer Biomet advisory board on rapid recovery, and CV received travel expenses from Stryker with no relevance to the present study. The remaining authors report no conflicts of interest related to this project. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2024.40185
Results
The study cohort included 2,756 patients with 1,267 primary THAs, 1,065 primary TKAs, and 424 primary UKAs. The mean age was 69 years and 58% were females (Table 4).
Table 4.
Patient demographics. Values are percentages unless otherwise specified
| Factor | Entire study cohort | Eligible patients n = 1,022 | Non-eligible patients n = 1,734 | ||
|---|---|---|---|---|---|
| DOS | Not DOS | DOS | Not DOS | ||
| Surgical procedure, n | 2,756 | 527 | 495 | 63 | 1,671 |
| THA | 1,267 | 213 | 223 | 20 | 846 |
| TKA | 1,065 | 188 | 184 | 21 | 615 |
| UKA | 424 | 126 | 88 | 22 | 210 |
| Mean age, years | 69 | 65 | 66 | 67 | 71 |
| Sex | |||||
| Female | 58 | 48 | 55 | 59 | 61 |
| Male | 42 | 52 | 45 | 41 | 39 |
| Mean body mass index | 29 | 27 | 29 | 28 | 30 |
| Cohabitation | |||||
| Cohabiting | 73 | 91 | 87 | 69 | 62 |
| Living alone | 27 | 9 | 13 | 31 | 38 |
| Mean CFS | 2.5 | 2.1 | 2.2 | 2.6 | 2.8 |
| Pharmacologically treated | |||||
| diabetes mellitus | 9 | 5 | 8 | 6 | 11 |
| heart disease | 58 | 48 | 51 | 51 | 64 |
| pulmonary disease | 26 | 11 | 12 | 13 | 34 |
DOS = discharged on the day of surgery.
CFS = Clinical Frailty Scale [25].
1,022 patients (37%, CI 35–39) were found eligible for discharge on day of surgery (Figure 1). The proportion of patients eligible ranged from 21% to 50% between centers and causes of not being eligible are presented in Figure 2. 52% (CI 49–55) of the eligible patients were discharged on the day of surgery, with a range of 24–62% between the centers (Figure 3). 92% of the eligible patients had start of surgery before 1 pm as intended according to the study protocol.
Figure 2.
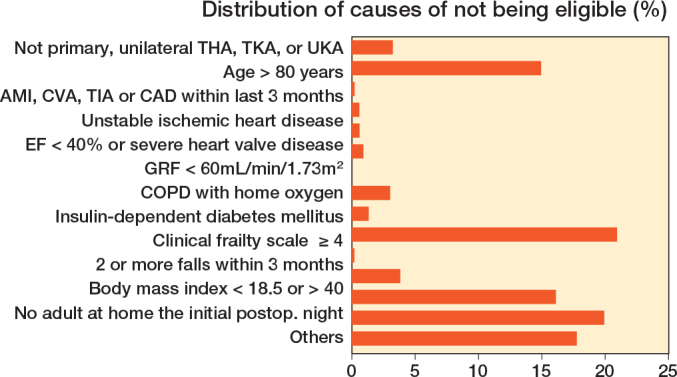
Causes of not being eligible for discharge on day of surgery.
AMI = acute myocardial infarction. CVA = cerebrovascular accident. TIA = transient ischemic attack. CAD = coronary atherosclerotic disease. EF = ejection fraction. GFR = glomerular filtration rate. COPD = chronic obstructive pulmonary disease. CFS = Clinical frailty scale. Others = e.g., cognitively impaired patient, elderly/ill cohabitant, requiring ferry transport to get home, etc.
Figure 3.

(Left panel) Patients found eligible for discharge on day of surgery on center level (A–G). (Right panel) Proportion of eligible patients discharged on the day of surgery on center level (A–G).
21% (CI 20–23) of all patients (eligible and non-eligible) were discharged on the day of surgery (range 10–31% between centers) (Figure 4). There was a statistically significant difference in the overall proportion of patients discharged on day of surgery between 2019 (control period 6%) and 2023 (study period 21%), with a difference of 15% (CI 13–17, P < 0.001). 36% of UKAs, 20% of TKAs, and 18% of THAs were discharged on day of surgery.
Figure 4.
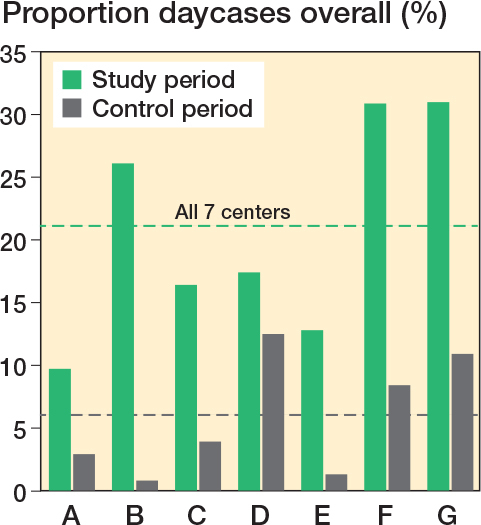
Overall discharge on day of surgery on center level (A–G) in the study period (September 1, 2022–February 28, 2023) versus the control period (July 1, 2019–December 31, 2019).
The distribution of patients discharged on the day of surgery was relatively constant during the 6-month implementation period.
Discussion
We aimed to describe the implementation of outpatient hip and knee arthroplasty in a multicenter public healthcare setting, and we found an increase in outpatient surgery from 6% at baseline to 21% during the implementation period of the study protocol. To our knowledge, this is the first multicenter study with a study protocol including well-defined eligibility criteria and discharge criteria from a public healthcare setting reporting the feasibility of multicenter implementation of outpatient hip and knee replacement.
Despite an increasing interest in outpatient surgery worldwide, the eligibility criteria are still debatable. In- and exclusion criteria in our study were based on previous data from outpatient surgery [16-17] as well as our previous multicenter data on the risk of complications after fast-track hip and knee arthroplasty [4].
52% of the eligible patients were discharged on the day of surgery, where previous prospective studies have reported huge variations in success from 24–99% [7-10,17-19]. There are several possible explanations for these variable results. First, the selection of patients in the studies varied and was not always based on well-defined in- and exclusion criteria [9,18,20-21]. Furthermore, some studies were performed in ambulatory day care center settings with very restrictive eligibility criteria including mainly healthy young patients [8,10]. Finally, previous study cohorts were rather small (n ≤ 200 patients) making generalizability and interpretation difficult [8-10,18].
In our population representing participants from all regions of the country, the frequency of patients found eligible for discharge on the day of surgery varied considerably between the centers. 5 of the centers receive mainly elective patients whereas 2 centers have both acute and elective patients on the same site. Furthermore, the individual surgeon’s interpretation of the protocol and the concept of discharge on day of surgery may play a role despite the pre-study educational program being instituted at all centers [13].
We also found important differences in the proportion of patients discharged on day of surgery among centers. Only 3 of the study centers (center D, F, G in Figure 4) had previous experience with discharge on day of surgery, and 2 of these centers improved considerably from about 10% at baseline to about 30% in the study period. 4 centers had no pre-study experience with discharge on day of surgery and 3 centers reached 10% of outpatient surgery with 1 center reaching 26%. Surprisingly, we did not observe any significant increase in the proportion discharged on day of surgery during the 6-month study period, requiring further study over a longer time period. Nevertheless, based on this initial data, we estimate it to be realistic to achieve an overall 30% discharge on day of surgery in our multicenter collaboration within the following years.
The overall frequency of patients discharged on day of surgery reached 21% in the implementation period of our study. In comparison, Coenders et al. reached 34% of 257 patients discharged on the day of surgery in their prospective study over 3.5 years. The proportion of patients meeting the inclusion criteria (40%) was at the same level as our study (37%), but they included only primary THAs from a single private center [7].
The strength of our study was the prospective design with a well-defined setup [13]. Furthermore, our study included data from a multicenter collaboration contributing about 40% of all annual primary hip and knee arthroplasties in Denmark [22,23] from all Danish regions and from a socialized healthcare setting, which may increase the generalizability of the results. The multicenter collaboration was originally established in 2009, and thus was already well-functioning before the implementation of the protocol for this study [15].
We acknowledge that time trends throughout the study period may have introduced confounding factors in our before-and-after analysis. Additionally, diverse logistical barriers at individual centers could have influenced our results, despite adherence to the same protocol, which included a pre-study educational program [13]. Further investigation of the center type aspect is warranted and a subject for upcoming studies. Another limitation of the study was that not all centers reached acceptable completeness of data in the REDCap database during the implementation period (Table 3, see Appendix). Reasons for incompleteness were primarily related to logistical challenges with implementation of the database on center level. A few patients also refused to provide informed consent to registration within the REDCap database, which might introduce selection bias.
The internal logistic problems have been solved with all centers having reached 90% data completeness after the implementation period. However, we also acknowledge that the overall frequency of patients discharged on day of surgery may be overestimated, as we have no information on patients not included in the database. Finally, our collaboration focuses not only on the speed of discharge, but also on the safety of the outpatient setup [24]. This important aspect will be secured in future studies by complete follow-up through the established obligatory health registers in Denmark. Nevertheless, our current study aimed to describe the feasibility of implementation of our study protocol for outpatient surgery and may provide valuable information for setting realistic goals when planning an outpatient protocol in other institutions.
Conclusion
During the implementation period we found it possible to perform outpatient hip and knee arthroplasty in 21% of patients in a multicenter public healthcare setting.
CV, TJ, MRA, MJB, SO, CCJ, HK, KG, and MLL are members of the Center for Fast-track Hip and Knee Replacement steering committee. The study protocol and guideline were planned at steering committee meetings. OD and CBJ undertook data gathering. OD and MLL drafted the manuscript. All authors reviewed the manuscript.
Handling co-editors: Bart Swierstra and Philippe Wagner
Acta thanks Nina Mathijssen for help with peer review of this manuscript.
References
- 1.Andreasen S E, Holm H B, Jorgensen M, Gromov K, Kjaersgaard-Andersen P, Husted H. Time-driven activity-based cost of fast-track total hip and knee arthroplasty. J Arthroplasty 2017; 32(6): 1747-55. doi: 10.1016/j.arth201612040. [DOI] [PubMed] [Google Scholar]
- 2.Bemelmans Y F L, Keulen M H F, Heymans M, Van Haaren E H, Boonen B, Schotanus M G M. Safety and efficacy of outpatient hip and knee arthroplasty: a systematic review with meta-analysis. Arch Orthop Trauma Surg 2022; 142(8): 1775-91. doi: 10.1007/s00402-021-03811-5. [DOI] [PubMed] [Google Scholar]
- 3.Mantel J, Ruppenkamp J W, Cantu M, Holy C. Total knee arthroplasty in the outpatient vs inpatient settings: impact of site of care on early postoperative economic and clinical outcome. J Orthop Surg Res 2023; 4; 18(1): 273. doi: 10.1186/s13018-023-03750-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petersen P B, Kehlet H, Jorgensen C C, Knee Replacement Collaborative Group. Improvement in fast-track hip and knee arthroplasty: a prospective multicentre study of 36,935 procedures from 2010 to 2017. Sci Rep 2020; 4; 10(1): 21233. doi: 10.1038/s41598-020-77127-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wainwright T W, Memtsoudis S G, Kehlet H. Fast-track hip and knee arthroplasty … how fast? Br J Anaesth 2021; 126(2): 348-9. doi: 10.1016/j.bja.2020.09.038. [DOI] [PubMed] [Google Scholar]
- 6.Rozell J C, Ast M P, Jiranek W A, Kim R H, Della Valle C J. Outpatient total joint arthroplasty: the new reality. J Arthroplasty 2021; 36(7S): S33-9. doi: 10.1016/j.arth.2021.02.030. [DOI] [PubMed] [Google Scholar]
- 7.Coenders M J, Mathijssen N M C, Vehmeijer S B W. Three and a half years’ experience with outpatient total hip arthroplasty. Bone Joint J 2020; 102-B(1): 82-9. doi: 10.1302/0301-620X102B1BJJ-2019-0045R2. [DOI] [PubMed] [Google Scholar]
- 8.Lovasz G, Aros A, Toth F, Faye J V, Malfa M L. Introduction of day case hip and knee replacement programme at an inpatient ward is safe and may expedite shortening of hospital stays of traditional arthroplasties. J Orthop Surg Res 2021; 16(1): 585. doi: 10.1186/s13018-021-02737-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parcells B W, Giacobbe D, Macknet D, Smith A, Schottenfeld M, Harwood D A, et al. Total joint arthroplasty in a stand-alone ambulatory surgical center: short-term outcomes. Orthopedics 2016; 39(4): 223-8. doi: 10.3928/01477447-20160419-06. [DOI] [PubMed] [Google Scholar]
- 10.Shi Y, Zhu P, Jia J, Shao Z, Yang S, Chen W, et al. Cost-effectiveness of same-day discharge surgery for primary total hip arthroplasty: a pragmatic randomized controlled study. Front Public Health 2022; 25(10): 825727. doi: 10.3389/fpubh2022825727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jensen C B, Troelsen A, Foss N B, Nielsen C S, Lindberg-Larsen M, Gromov K. 10-year evolution of day-case hip and knee arthroplasty: a Danish nationwide register study of 166,833 procedures from 2010 to 2020. Acta Orthop 2023; 94: 178-84. doi: 10.2340/17453674202311961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wainwright T W. The current status of daycase hip and knee arthroplasty within the English National Health Service: a retrospective analysis of hospital episode statistics data. Ann R Coll Surg Engl 2021; 103(5): 324-31. doi: 10.1308/rcsann20207142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lindberg-Larsen M, Varnum C, Jakobsen T, Andersen M R, Sperling K, Overgaard S, et al. Study protocol for discharge on day of surgery after hip and knee arthroplasty from the Center for Fast-track Hip and Knee Replacement. Acta Orthop 2023; 94: 121-7. doi: 10.2340/17453674.2023.11636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benchimol E I, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med 2015; 12(10): e1001885. doi: 10.1371/journal.pmed1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sorensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449-90. doi: 10.2147/CLEPS91125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Center for Fast Track – Hip and Knee Replacement. Available from: www.fast-track.health. [Google Scholar]
- 16.Berend K R, Lombardi A V, Berend M E, Adams J B, Morris M J. The outpatient total hip arthroplasty: a paradigm change. Bone Joint J 2018; 100-B(1 Supple A): 31-5. doi: 10.1302/0301-620X.100B1.BJJ-2017-0514.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gromov K, Kjaersgaard-Andersen P, Revald P, Kehlet H, Husted H. Feasibility of outpatient total hip and knee arthroplasty in unselected patients. Acta Orthop 2017; 88(5): 516-21. doi: 10.1080/1745367420171314158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goyal N, Chen A F, Padgett S E, Tan T L, Kheir M M, Hopper R H, et al. A multicenter, randomized study of outpatient versus inpatient total hip arthroplasty. Clin Orthop Relat Res 2017; 475(2): 364-72. doi: 10.1007/s11999-016-4915-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmidt A M, Garval M, Gromov K, Holm C, Larsen J R, Runge C. Feasibility, safety, and patient-reported outcomes 90 days after same-day total knee arthroplasty: a matched cohort study. Acta Orthop 2022; 93: 509-18. doi: 10.2340/1745367420222807. [DOI] [PubMed] [Google Scholar]
- 20.Darrith B, Frisch N B, Tetreault M B, Fice M P, Culvern C N, Della Valle C J. Inpatient versus outpatient arthroplasty: a single-surgeon, matched cohort analysis of 90-day complications. J Arthroplasty 2019; 34(2): 221-7. doi: 10.1016/j.arth201810015. [DOI] [PubMed] [Google Scholar]
- 21.Verdier N, Boutaud B, Ragot P, Leroy P, Saffarini M, Nover L, et al. Same-day discharge to home is feasible and safe in up to 75% of unselected total hip and knee arthroplasty. Int Orthop 2022; 46(5): 10.19-27. doi: 10.1007/s00264-022-05348-7. [DOI] [PubMed] [Google Scholar]
- 22.Danish Knee Arthroplasty Register (DKR). , 2021 (B) National Annual Report. Available from: URL: http://www.rkkp.dk. [Google Scholar]
- 23.Danish Hip Arthroplasty Register (DHR). , 2021 (B) National Annual Report. Available from: URL: http://www.dhr.dk. [Google Scholar]
- 24.Joshi G P, Kehlet H. Enhanced recovery and same-day discharge hospital stay: speed versus safety? Br J Surg 2023; 110(12): 1644-5. doi: 10.1093/bjs/znad222. [DOI] [PubMed] [Google Scholar]
- 25.Nissen S K, Fournaise A, Lauridsen J T, Ryg J, Nickel C H, Gudex C, et al. Cross-sectoral inter-rater reliability of the clinical frailty scale: a Danish translation and validation study. BMC Geriatr 2020; 20(1): 443. doi: 10.1186/s12877-020-01850-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Physicians RCo . National Early Warning Score (NEWS) 2: standardising the assessment of acute-illness severity in the NHS. Updated report of working party 2017. Available from: file:///C:/Users/iby8fi/AppData/Local/Temp/MicrosoftEdgeDownloads/20c21027-af83-489a-905b-0ff54dc6dff9/NEWS2%20final%20report_0_0.pdf. [Google Scholar]



